Prostate cancer testing and diagnosis
Getting tested for prostate cancer can feel overwhelming and daunting. With waits for NHS referrals and the emotional toll of possible results, it’s normal to experience anxious.
Screening for prostate cancer involves a range of tests and decisions, and this guide is here to help you.
Whether you’re seeking peace of mind or already experiencing symptoms, understanding what to expect helps you feel more in control. Here, we’ll cover everything from the PSA blood test and GP referrals to cutting-edge diagnostics like multiparametric MRI (mpMRI) scans and biopsies.
Why testing for prostate cancer matters
Early detection
Early detection of prostate cancer is key to improving outcomes. Identified in its early stages, prostate cancer is often localised, offering wider treatment options and higher survival rates.
Being proactive during this process can make a difference. By understanding the available options, patients can ask the right questions and potentially fast-track decisions.
Useful resource links

Preparing for your appointment
Being well-prepared for a doctor’s appointment helps you make the most of your consultation, to help get the answers and support you need.
Ask the right questions
Here are some helpful questions to consider:
- The benefits and potential risks of prostate cancer screening tests, like the PSA test?
- Based on personal and family history, what are my risk factors for developing prostate cancer?
- How different types of prostate cancer are diagnosed, what does the process involve?
- Treatment options available if I am diagnosed with prostate cancer, and what side effects should I be aware of?
- How often should I undergo prostate cancer screening, and screening tests recommended for me?
- Common signs and symptoms of prostate cancer, and when to seek further medical advice?
What to bring to your appointment
- Detailed medical history, including previous prostate issues or cancer diagnoses.
- List of medications and supplements you are taking.
- Family’s medical history, including cases of prostate cancer or breast cancer.
- Results from previous prostate cancer screening tests.
- Any specific concerns you want to discuss.
Being proactive and prepared helps you take control.
PSA blood test and GP referral
What is a PSA test?
PSA tests measure prostate-specific antigen (PSA) levels in your blood. PSA is a protein produced by the prostate gland. Elevated PSA levels can indicate prostate cancer. It is also worth knowing that PSA isn’t always an indication of prostate cancer as elevated levels can also arise from benign prostatic hyperplasia (enlarged prostate), a urinary infection or even recent ejaculation.
What are the pros and cons of PSA testing?
Pros:
- Detect prostate issues early, often before symptoms occur.
- Raised PSA could indicate a fast-growing cancer requiring immediate treatment.
Cons:
- High PSA results can lead to unnecessary worry, as it doesn’t confirm cancer.
- False positives and negatives are possible, leading to overdiagnosis or missed detection.
What to expect at a PSA test?
PSA testing is a simple blood test conducted at your GP practice. If your PSA results are above average for your age group, your GP may recommend further investigations, such as an mpMRI scan or a biopsy.
Age-related PSA thresholds:
- 40–49 years: Above 2.5 ng/ml is considered high.
- 50–59 years: Above 3.5 ng/ml is considered high.
- 60–69 years: Above 4.5 ng/ml is considered high.
GPs may also perform a digital rectal examination (DRE), which involves feeling the prostate to check for any irregularities.
https://www.cancerresearchuk.org/about-cancer/tests-and-scans/prostate-specific-antigen-psa-test
For more details, visit these resources:
Digital Rectal Exam (DRE)
A digital rectal exam (DRE) is a simple yet important test that plays a key role in prostate cancer screening and diagnosis. Understanding what to expect from a DRE can help ease any anxiety and highlight its value in detecting prostate cancer early.
What is a DRE?
During a digital rectal exam, your doctor inserts a gloved, lubricated finger into your rectum to feel the prostate gland. This quick and straightforward test allows the doctor to check for any unusual lumps, hard areas, or changes in the size and texture of the prostate that could indicate prostate cancer or other prostate conditions.
While a DRE alone cannot diagnose prostate cancer, it is an essential part of the screening process, especially for men at higher risk—such as those with a family history of prostate cancer. If your doctor detects any abnormalities during the exam, they may recommend further tests, such as a PSA test, MRI scan, or even a prostate biopsy, to help diagnose prostate cancer more accurately.
A DRE can also help identify other prostate problems, such as benign prostatic hyperplasia (BPH) or prostatitis, which can cause urinary symptoms like difficulty urinating or increased frequency.
Combining a DRE with other prostate cancer screening tests, such as the PSA blood test and advanced imaging tests, increases the chances of detecting prostate cancer early—when it is most treatable.
Multiparametric MRI scans
What is mpMRI?
Multiparametric MRI (mpMRI) scans are advanced imaging tests recommended for suspected prostate cancer. They provide high-resolution images of the prostate gland and surrounding tissues, helping doctors identify abnormal areas that may need further investigation
Why it’s important?
The mpMRI scan often helps patients avoid unnecessary biopsies. If no abnormalities are detected, a biopsy may not be required, sparing patients from an invasive procedure.
What should I expect from the scan?
An mpMRI scan is painless and usually takes 30–45 minutes. You’ll lie on a table that moves through the MRI machine while it takes detailed images of your prostate. Some scans may involve a contrast dye injected into your bloodstream for clearer images.
Further reading on mpMRI can be found at Prostate Cancer UK.
Prostate biopsy procedures
When is a biopsy needed?
If an mpMRI scan shows suspicious areas or your PSA remains consistently elevated, a biopsy will likely be recommended to check for cancerous prostate tissue.
What are the common types of biopsy?
1. Transperineal Biopsy
● Tissue is sampled through the skin between the scrotum and rectum.
○ Safer with less infection risk compared to traditional methods.
2. Transrectal Ultrasound-Guided Biopsy (TRUS)
● Tissue is collected via the rectum using an ultrasound probe.
○ Often more accessible, but higher infection risk.
3. Template Mapping Biopsy
● Highly precise biopsy method. Suitable for complex or unclear cases.
How should I prepare for the procedure?
Before the biopsy, your doctor will provide instructions on fasting, hydration, and stopping certain medications. A local or general anaesthetic is used to ensure minimal discomfort.
What should I expect afterwards?
Some common side effects include light bleeding in the urine or semen, soreness in the biopsy area, or short-term difficulty urinating. Results usually take 1–2 weeks and are reviewed during a multidisciplinary team (MDT) meeting to plan next steps if cancer is confirmed.
For a detailed guide, visit Cancer Research UK’s Biopsy Resource.
What happens after testing?
MDT review and next steps
Once your biopsy and other tests are complete, a MDT evaluates your case. They will determine the stage of the cancer (localised, advanced, or metastatic) and discuss treatment options, such as active surveillance, radiation therapy, or surgery.
Ask questions
Never hesitate to ask your medical team questions about your results, treatments, or additional tests you may require.

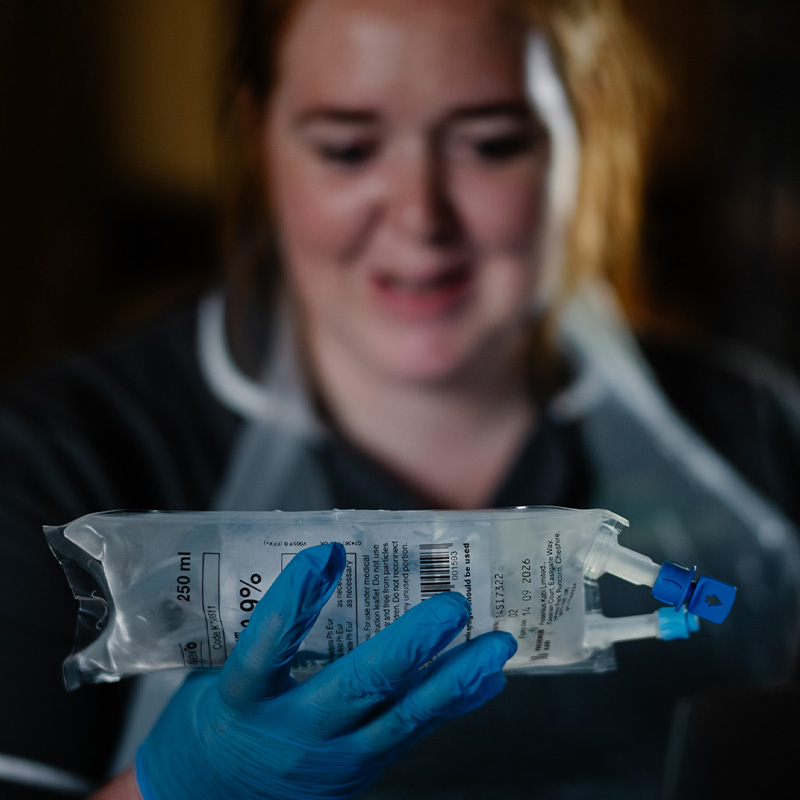
We know the benefits of cancer care at home
Our specialist cancer services ensure private medically insured and self-paying patients who want an alternative to hospital can start their treatment faster. We consider all cancer treatments, including those not currently available in hospitals.

Looking for more information?
We’ve worked with thousands of patients, and we know you’ll have a lot of questions.
If you’re ready to talk to us to discuss your options, fill out the form below and we’ll be in touch quickly.
If your enquiry is urgent please call 0345 2636 123 (England and Wales) or 0345 2636 135 (Northern Ireland and Scotland).
Your guide to prostate cancer treatment
A prostate cancer diagnosis can be overwhelming. Rest assured, you’re not alone, and there are many options for managing the condition and tailoring treatment to suit your individual needs.
Our guide is here to help you understand private prostate cancer treatment and the main treatment options available.