Optimising peripheral intravenous catheter insertion and management in out-of-hospital settings: addressing patient and technical factors, enhancing nurse competency, and promoting evidence-based practices for improved outcomes
Leoni Walker, Lead Nurse Rare Disorders, Immunoglobulins and IV Therapies, Lloyds Clinical
Background
Peripheral intravenous catheter (PIVC) insertion is a fundamental procedure in out-of-hospital patient care, routinely employed for the administration of fluids, medications, and other essential therapies. Despite being a common intervention, difficulties with PIVC insertion—particularly multiple failed attempts—remain a persistent challenge. These difficulties are commonly referred to as difficult intravenous access (DIVA), a term encompassing a range of patient- and procedure-related factors that hinder successful cannulation on the first attempt. These failures can cause patient discomfort, delay treatment, increase the risk of complications, and place additional strain on healthcare resources [1].
At Lloyds Clinical, successful venous access is achieved in the majority of cases; however, a pattern of first-attempt failures has emerged across certain patient groups. These incidents not only impact the quality of patient care but also affect service efficiency and staff workload. Through routine service evaluations and clinical audits, a significant gap was identified in our understanding of the underlying causes of difficult intravenous access (DIVA) within our population.
This quality improvement project was initiated in response to these findings. By investigating patient-specific and procedural factors contributing to insertion failures, the goal is to enhance both the success rates of PIVC insertion and the overall patient experience. Addressing this challenge is essential to ensuring safe, effective, and patient-centred care in out of hospital settings.
Aim and methods
This study explores the challenges associated with peripheral intravenous catheter (PIVC) placement in out-of-hospital settings. PIVC insertion is the most frequently performed invasive procedure in healthcare and is essential for the delivery of many therapies [2].
At Lloyds Clinical, these therapies include treatments for lysosomal storage disorders, systemic anti-cancer therapy (SACT), intravenous antibiotics, and a range of therapies for rare and complex conditions.
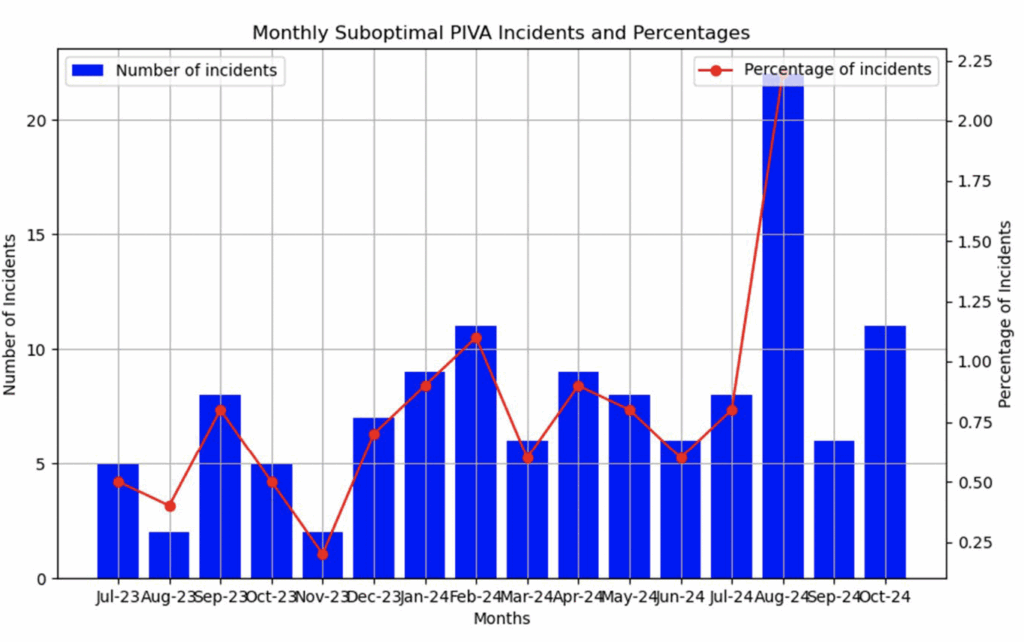
A retrospective observational study was conducted over a 17-month period, from July 2023 to November 2024, encompassing 16,872 nursing visits. The primary aim was to identify instances of suboptimal PIVC insertion and to examine contributing factors associated with reduced first-attempt success.
At Lloyds Clinical, venous access is classified as unsuccessful if the visiting nurse is unable to establish a functioning peripheral intravenous line within four attempts. This limit was established in line with the Vessel Health and Preservation Framework guidance [4]. Additionally, any visit requiring more than one attempt is routinely audited. This process supports ongoing clinical safety monitoring and contributes to continuous improvement of the patient experience.
Analysis of suboptimal venous access
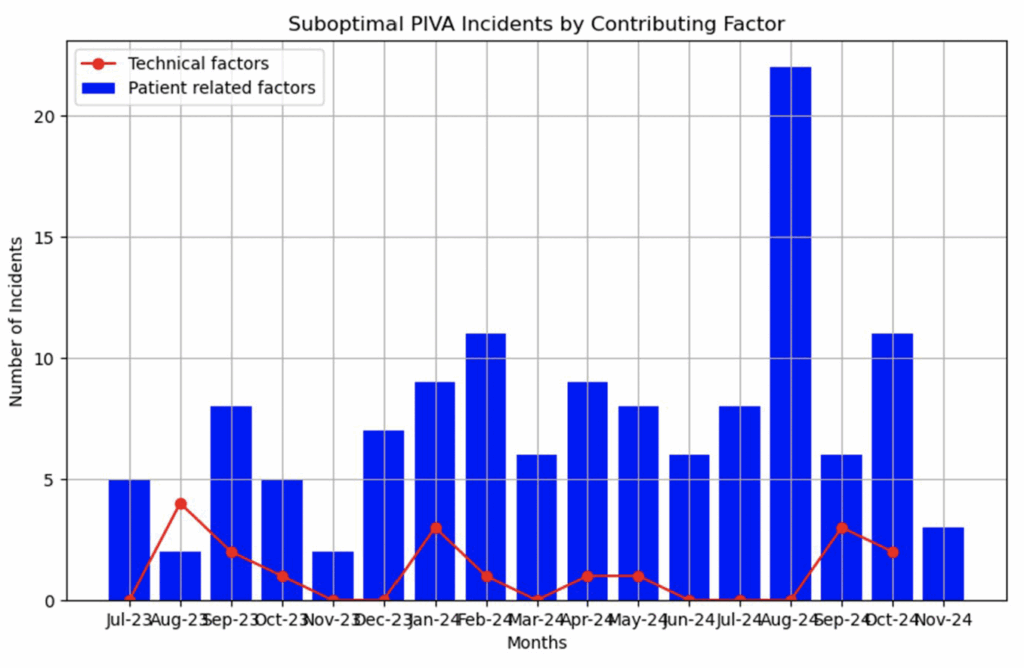
To better understand patterns in failed or suboptimal peripheral intravenous access (PIVA), incidents were categorised into two primary themes:
1. Patient-related anatomical and physiological factors:
• Small or poorly visible veins
• Obesity or scarring from previous procedures
• Poor circulation, dehydration, or oedema
• Age-related vein changes or anxiety impacting vein dilation
2. Technical factors:
• Suboptimal insertion technique
• Equipment-related issues
• Lack of clinician confidence or experience
Across the 140 incidents of suboptimal PIVA recorded, 128 cases (92.75%) were attributed to patient-related factors. The remaining 12 cases (7.25%) were linked to technical issues, the most common theme being reduced nurse confidence during the procedure.
Conclusions
Failed venous access is frequently linked to patient-specific anatomical and physiological factors, such as poor vein visibility and prior medical interventions which aligns with the findings of this study. A thorough evaluation of current practices revealed significant gaps—not only in our clinical strategies but also in patient awareness and engagement. Research consistently shows that well-informed patients contribute meaningfully to improved outcomes; however, there remains a lack of theory-based, patient-focused interventions [3]. In response, an evidence-based patient education leaflet was developed, now implemented across all adult therapy groups at Lloyds Clinical. This resource empowers patients with practical, actionable steps—such as maintaining hydration, keeping warm, and employing anxiety-reducing techniques—that enhance vein visibility and reduce insertion-related complications.
Recognising the need to support younger patients, Lloyds Clinical will now develop a paediatric version tailored to children and their families, promoting confidence and cooperation during procedures. Importantly, these educational tools also serve to support clinical staff by reinforcing up-to-date, evidence-based venous access techniques. By addressing both patient and staff knowledge gaps, this initiative aims to improve success rates, reduce patient anxiety, and elevate care quality in out-of-hospital settings. Ongoing monitoring and feedback will ensure these strategies continue to evolve in line with best practice and patient needs.
References
1. Simonsmeier, B.A., Flaig, M., Simacek, T., & Schneider, M. (2021). What sixty years of research says about the effectiveness of patient education on health: A second-order meta-analysis. Health Psychology Review, 16(3), 450–474. https://doi.org/10.1080/17437199.2021.1967184
2. Bahl, A., Johnson, S., Alsbrooks, K., Mares, A., Gala, S., & Hoerauf, K. (2021). Defining difficult intravenous access (DIVA): A systematic review. Journal of Vascular Access. Advance online publication. https://doi.org/10.1177/11297298211059648
3. Thompson, J., Steinheiser, M.M., Hotchkiss, J.B., Davis, J., DeVries, M., Frate, K., Helm, R., et al. (2024). Standards of care for peripheral intravenous catheters: Evidence-based expert consensus. Journal of the Association for Vascular Access, 29(3), 15–26. https://doi.org/10.2309/JAVA-D-24-00011
4. Moureau, N. L. (Ed.). (2019). Vessel Health and Preservation: The Right Approach for Vascular Access. Springer. https://doi.org/10.1007/978-3-030-03149-






