Understanding lung cancer treatment
Whether you have non-small cell lung cancer, small cell lung cancer, or another type, such as squamous cell carcinoma, your care team aims to treat lung cancer with the best treatment plan for your case.
This guide will walk you through the treatment options available for lung cancer today, from surgery and chemotherapy to targeted therapies, immunotherapy, and home care solutions.
Understanding your lung cancer diagnosis
Creating an effective treatment plan begins with understanding the specifics of your lung cancer diagnosis. When lung cancer is identified, whether through imaging tests, lung cancer screening, or tissue samples from a biopsy, your healthcare team assesses several key factors to diagnose lung cancer and determine the right approach.
Cancer type
Lung cancer primarily falls into two main groups:
- Non-small cell lung cancer (NSCLC) – the most common type of lung cancer, including squamous cell carcinoma, accounts for most lung cancers and often grows more slowly.
- Small cell lung cancer (SCLC) – a less common type, also known as small cell carcinoma, tends to spread more rapidly and may be more aggressive. Some lung cancer cases may also include rare types, such as large cell carcinoma.
Stage of cancer
Imaging tests like CT scans, PET scans, or magnetic resonance imaging help determine if you have early-stage cancer, advanced disease, or metastatic lung cancer. The presence of cancerous cells or malignant cells in lymph nodes or other tissues is also carefully assessed.
Early-stage lung cancer is typically localised and may be suitable for surgery and other treatments. Advanced-stage or metastatic lung cancer (when the cancer has spread to other organs) usually requires systemic therapies to treat the cancer effectively.
Biomarker testing
Your team may perform biomarker or genetic testing using tissue samples to uncover specific features of your lung cancer cells or tumour cells. Identifying biomarkers such as EGFR, ALK, or PD-L1 is important for selecting targeted therapies, targeted therapy drugs, or immunotherapy. Such precision medicine helps match the best treatment options to your unique cancer.
Participating in clinical trials, including those run by organisations such as the National Cancer Institute or the National Cancer Institute’s affiliated groups, may offer access to cutting-edge lung cancer treatments, targeted treatments, or alternative medicine approaches.
Surgery for lung cancer
If lung cancer is detected at an early stage, health professionals may recommend surgery to remove the lung cancer and the surrounding affected lung tissue. Surgical treatment is also used for some cases of recurrent or isolated metastatic lung cancer.
Types of surgery
- Lobectomy – The most common surgery for both non-small cell lung cancer and some small cell lung cancer cases, which removes the lobe containing the primary tumour or abnormal tissue.
- Pneumonectomy – Removes the entire lung if cancer cells or malignant cells are located centrally, in multiple lobes, or if the cancer has spread throughout one lung.
- Segmentectomy/Wedge Resection – Removes only the tumour and a small portion of the lung tissue. A wedge resection is often performed when preserving lung function is important for lung cancer patients with reduced lung function or early-stage disease.
Lymph node removal
During surgery, nearby lymph nodes (including mediastinal lymph nodes) may also be removed and examined to see if cancer cells have spread. This step helps guide further treatment, such as chemotherapy or palliative radiotherapy, if cancer is found in the lymph nodes or surrounding tissues.
Advancements in techniques, such as minimally invasive surgery or robotic-assisted procedures, help protect healthy tissue and can result in shorter recovery times for lung cancer.
Chemotherapy for lung cancer
Chemotherapy is one of the most common treatments for lung cancer, used to kill cancer cells, destroy cancer cells, or shrink tumours before or after surgery.
Types of chemotherapy
- Adjuvant chemotherapy – Given after surgery to destroy any remaining cancerous cells in the lung tissue or lymph nodes, reducing the risk of recurrence.
- Neo-adjuvant chemotherapy – Administered before surgery with the aim of shrinking the primary tumour and making it easier to remove the lung cancer with clear margins.
- Palliative chemotherapy – Used for advanced or metastatic lung cancer to relieve symptoms, improve quality of life, or slow cancer spread in lung cancer patients who may not be candidates for surgery.
Chemotherapy treatments may be combined with other treatments, such as radiation therapy, targeted therapies, or immunotherapy drugs, based on the type of lung cancer and other risk factors.
Managing side effects
Your healthcare team will discuss ways to manage side effects, protect healthy tissue, and maintain your overall health. Blood tests and imaging tests monitor how well you tolerate chemotherapy and detect any effects on lung function, as well as on your immune system. Complementary and alternative medicine can also provide support for symptom relief.
Targeted therapy
Targeted therapies are designed to treat lung cancer by attacking specific cancer cells or molecules (such as EGFR mutations or ALK rearrangements) found in your lung cancer diagnosis.
Biomarker and genetic targeting
Targeted therapy drugs, such as tyrosine kinase inhibitors, may be recommended if your lung cancer cells have genetic changes that these anti-cancer drugs can block. These therapies are most often used for non-small cell lung cancer or some metastatic lung cancer cases. Clinical trials continue to explore new targeted treatments that may further improve survival rates.
Targeted therapy typically causes fewer side effects compared to chemotherapy, as it works against abnormal tissue or cancerous cells while sparing more normal cells.

Immunotherapy
Immunotherapy drugs leverage your own immune system to identify and attack cancer cells in the body. For many cancer patients, especially those with metastatic or advanced lung cancer, immunotherapy represents a new and effective approach to treating lung cancer.
How it works
By interrupting the immune “checkpoints” that allow tumour cells to evade the immune system, these treatments help the body destroy cancer cells. Immunotherapy can be given alone or combined with chemotherapy, radiation therapy, or targeted therapies to increase the effectiveness for certain lung cancer cases.
What to expect
Immunotherapy is administered through intravenous infusions, typically in a hospital or outpatient setting. Your care team will closely monitor for side effects, as immune reactions can sometimes impact lung or other tissue, but prompt management by health professionals ensures your safety.

Radiation therapy
Radiation therapy is a key treatment for lung cancer, especially when surgery is not possible, or to relieve symptoms in metastatic or advanced disease.
- Stereotactic Body Radiation Therapy (SBRT) delivers a precise, high dose of radiation to kill cancer cells in small or early-stage tumours, while minimising impact on healthy tissue and adjacent organs.
- Radiation can be used as palliative radiotherapy to relieve pain (such as chest pain, bone pain) or other symptoms when lung cancer has spread.
Radiation oncologists work with your care team to create a tailored plan based on tumour location, cancer stage, and your general health.
Other lung cancer treatments
Treatment options for lung cancer are expanding through ongoing research and clinical trials. In addition to standard therapies, your team may consider:
- Photodynamic therapy: A treatment using laser light and medication to treat early-stage tumours or cancerous cells on the surface of the airways.
- Laser therapy: Laser light can help shrink tumours or relieve blockages in airways to relieve symptoms such as breathing difficulties.
- Biological therapies/Complementary and alternative medicine: Supportive approaches may assist in managing symptoms or side effects and improve quality of life for lung cancer patients.
Your team will also offer guidance about complementary or alternative medicine, which should be discussed alongside your medical treatments.
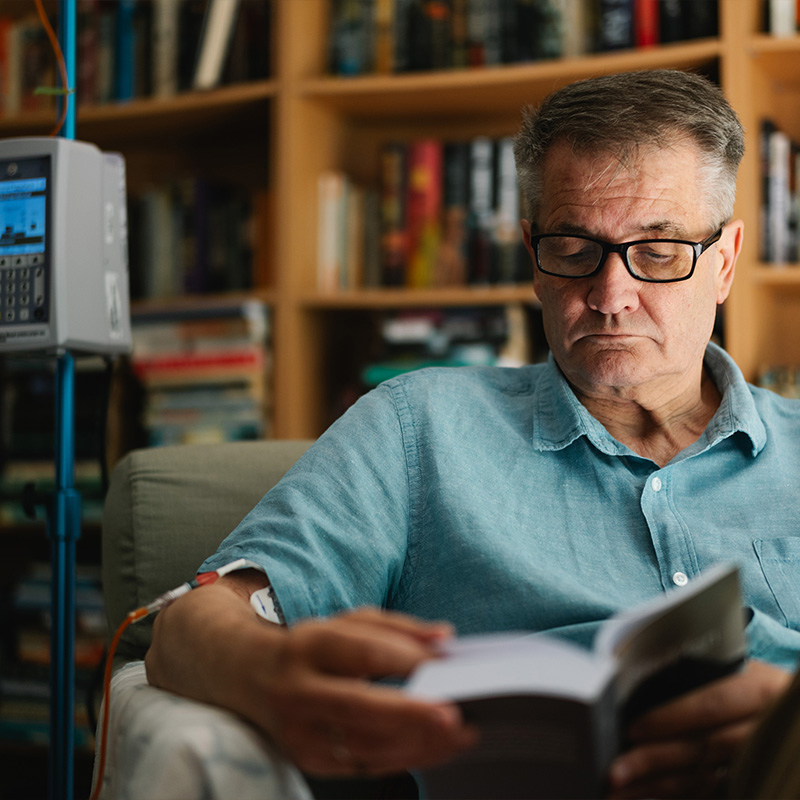
Home-based cancer treatment options
Many therapies, including chemotherapy, immunotherapy, and symptom management, can be safely delivered at home. Home-based care helps relieve pain, manage symptoms, and reduce the emotional and physical strain of frequent hospital visits. All treatments at home follow strict clinical protocols, and support lines ensure any concerns are addressed immediately, with direct communication to your consultant or chest physicians.
Benefits of treatment at home include:
Comprehensive support for your treatment journey
Treating lung cancer is about more than fighting malignant cells. Your multidisciplinary team includes surgeons, medical oncologists, radiation oncologists, and specialist nurses, all focused on every aspect of your care, body, mind, and family.
Addressing side effects
From optimising nutrition (including a healthy diet) to managing anti-cancer treatments and maintaining lung function, you’ll receive guidance for every step. Physiotherapy and psychological support are readily available to help you feel your best throughout your treatment plan.

Emotional and family support
Lung cancer affects not only the patient but also loved ones. Counsellors, peer support programmes, and information about clinical trials or complementary therapies are part of your support system.
Looking for more information?
We’ve worked with thousands of patients, and we know you’ll have a lot of questions.
If you’re ready to talk to us to discuss your options, fill out the form below and we’ll be in touch quickly.
If your enquiry is urgent please call 0345 2636 123 (England and Wales) or 0345 2636 135 (Northern Ireland and Scotland).
We know the benefits of cancer care at home
Our specialist cancer services ensure private medically insured and self-paying patients who want an alternative to hospital can start their treatment faster. We consider all cancer treatments, including those not currently available in hospitals.

Your guide to lung cancer treatment
Navigating a lung cancer diagnosis or understanding early-stage lung cancer and advanced disease can be daunting.
This guide brings together key information about lung cancer and its development, helping you recognise symptoms, explore lung cancer screening and diagnostic tools, and consider your treatment options.