Sepsis: What you need to know and do – Important advice for patients
Mary Williamson, Lead Nurse Home Parenteral Nutrition, Lloyds Clinical
Leoni Walker, Lead Nurse Rare Disorders, Immunoglobulins and IV Therapies, Lloyds Clinical
Jade Mickelsen, Lead Nurse Oncology, Lloyds Clinical
Natalie Mounter, Lead Nurse Infection Prevention and Control, Lloyds Clinical
Pam Donaghy – Lead Nurse, Training and Education, Lloyds Clinical
What is Sepsis?
Sepsis is a life-threatening condition that occurs when the bodies’ response to an infection becomes uncontrolled. Instead of fighting just the infection, the immune system overreacts and begins to damage the patients’ bodies’ own tissues and organs.
Sepsis can be difficult to recognise, especially in its early stages, but early detection and treatment are critical. It can affect people of all ages, including both adults and children.
Certain medications, medical devices, or long-term health conditions may increase a person’s risk of developing sepsis. However, anyone can develop sepsis, even those who are otherwise healthy so it’s important that everyone is aware of the signs and symptoms.
If you or someone you care for is feeling very unwell with signs of infection, it’s important to seek medical help without delay.
If your treatment or medical device increases your risk of developing sepsis, your healthcare team will provide you with specific guidance to help you stay safe and know what to look out for.
Recognising the signs of sepsis
Sepsis can present with a wide range of symptoms, and some may be subtle.
Common signs and symptoms
Fever or low temperature and shivering.
Confusion or slurred speech.
Difficulty breathing or fast breathing.
Clammy and sweaty skin or skin that is mottled and discoloured.
Extreme body pain or discomfort.
High heart rate, weak pulse, or low blood pressure.
Low urine output.
Symptoms in children
Fast breathing.
Convulsions.
Pale skin.
Lethargy or difficulty waking up.
Feeling cold to the touch.
The UK Sepsis Trust offers a helpful symptom checker, and you can also find reliable information on the NHS website. Home – The UK Sepsis Trust and Symptoms of sepsis – NHS
It’s important to remember that sepsis doesn’t look the same in everyone. Symptoms can vary from person to person, so knowing the signs and seeking medical advice promptly is essential.
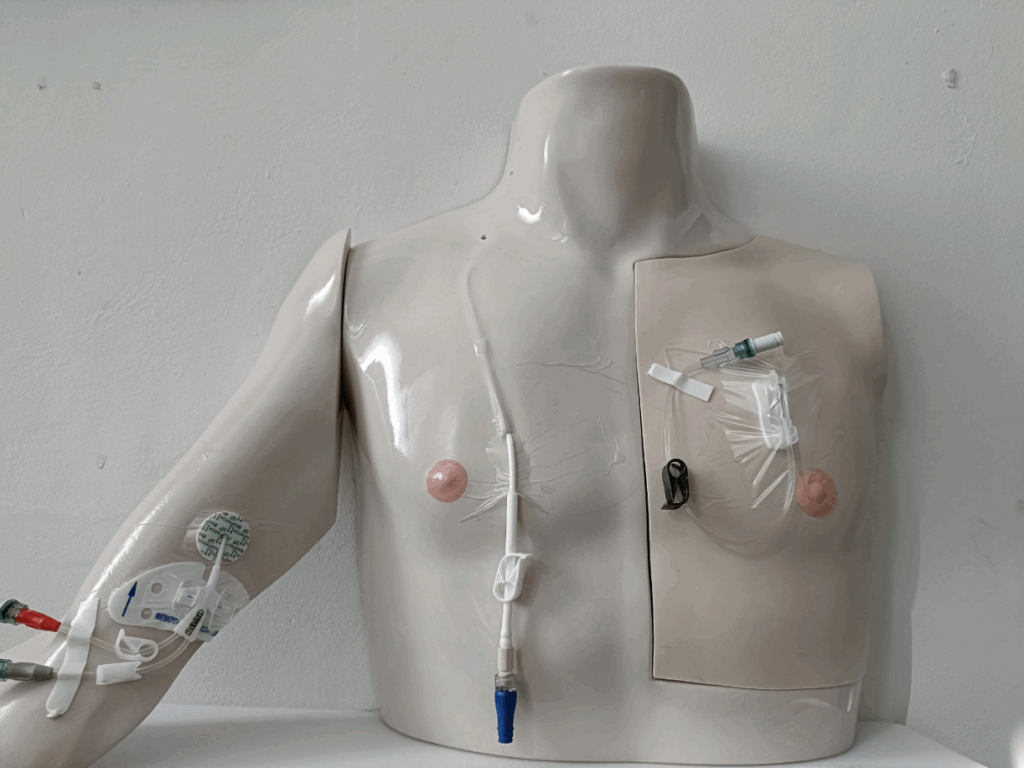
You or your loved one may have a central venous access device to enable treatments to be delivered safely. These come in many forms, from Peripherally inserted central catheters (PICC), Central Venous Catheter (CVC) or a totally implanted port-a-cath (port). You may be more familiar with them as their brand name.
Figure 1 – from left to right – PICC, CVC & PORT
As well as being aware of the signs of sepsis, following good care practices for your central venous access device (CVAD) can reduce your risk of developing a CVAD (which may be referred to as a line) associated infection.
Always follow aseptic non-touch technique (ANTT) when handling your CVAD. Avoid touching the key parts of your equipment and keep the end of your CVAD away from areas such as stomas, fistulas, or surgical wounds, where there may be a higher risk of contamination.
Before accessing your line, wash your hands thoroughly and follow the care protocols provided by your hospital team.
If a healthcare professional is handling your CVAD and you’re unsure about their technique, it’s okay to speak up or ask questions. This is your device, and it plays a vital role in keeping you well and out of hospital. Your involvement in its care is both welcome and important.
The World Health Organisation have a helpful guide to handwashing which can be accessed here: New_HandWash_Poster. They also have guidance on when its ok to use alcohol gel as a cleanser instead of hand washing New_HandRub_Poster.
Home Parenteral Nutrition
You or your loved one will be taught to monitor your temperature. If your temperature is 38°C or above, you should not administer your parenteral nutrition. If you have already commenced your infusion, this should be stopped. You will need to attend the hospital for a clinical review, to have blood tests taken.
In most cases, blood samples (known as cultures) will be taken both from a vein in your arm (peripheral) and from your central venous access device. Testing samples from both sites helps the medical team determine whether an infection is present and if your central line may be the source.
If you have other medical devices in place, such as a urinary catheter, surgical wound dressing, or enteral feeding device, additional samples may also be taken from these sites to help identify the cause of infection.
It’s important to know that a low temperature can also be a sign of sepsis. If you feel unwell or notice any symptoms – such as shivering or shaking after your infusion has started – please stop your pump and contact us straight away. One of our nursing team members will talk you through the next steps and ensure you get the support you need.
Oncology
Some cancer treatments, such as chemotherapy, immunotherapy, and certain targeted therapies, can temporarily weaken your immune system. This makes it harder for your body to fight infections, meaning that even a mild infection could become serious very quickly.
You will be given a SACT Alert Card with important emergency contact numbers. Please always carry this card with you.
Even if you feel well, a change in your body temperature can be an early sign of a serious infection. It is vital to check your temperature every day during treatment. Call the 24-hour advice line immediately if your temperature is 37.5°C or higher, or below 36.0°C, as both high and low readings can be signs of neutropenic sepsis, which requires urgent medical attention.
If this happens, phone the emergency number on your SACT Alert Card straight away. You may be asked to come to the hospital or a specialist triage unit for urgent assessment. Do not wait to see if your temperature improves – acting quickly could save your life.
Always keep your SACT Alert Card with you and ensure you have a working thermometer at home. If you are ever unsure, call for advice. Your safety is our top priority, and your oncology nursing team is here to support you at every step of your treatment.
Rare Disorders
If you or a loved one develops sepsis, or is being assessed for possible sepsis, it is vital to know how to manage your treatment safely. If you have a fever, feel very unwell, or suspect sepsis, do not start or continue your infusion. Having treatment during an infection can increase the risk of side effects and may delay urgent medical care.
Always tell the doctors and nurses looking after you that you are receiving treatment for a rare disorder, and let them know the name of your therapy, such as enzyme replacement therapy. This information helps them make the right decisions for your care.
Do not restart your treatment on your own after an infection. Speak to your specialist metabolic or genetics team first. Once you are stable and have recovered, they will advise you on when and how it is safe to begin treatment again. If our Lloyds Clinical nursing team support you with your treatment, they will liaise with your prescribing team to ensure we are giving you the correct care.
Immunoglobulins
If you are on regular immunoglobulin treatment, it is important to know what to do if you become unwell with an infection or think you may have sepsis. Do not give yourself an infusion if you have a fever, feel acutely unwell, or suspect sepsis, as treatment during an infection can increase side effects and make it harder to recognise early warning signs.
If you think you may have sepsis, pause your treatment and seek urgent medical help immediately by calling 999 or going to A&E. Always tell the doctors and nurses caring for you that you are on immunoglobulin therapy. Do not restart treatment on your own after an infection; wait until you have spoken with your immunology team. Once you are stable and your infection has been treated, they will advise you when it is safe to resume. If our Lloyds Clinical nursing team support you with your treatment, they will liaise with your prescribing team to ensure we are giving you the correct care.
Remember, sepsis is a medical emergency. Prioritise urgent care first – your treatment can be restarted later with guidance from your specialist team.
Injectable Medication (Biologic and Non-Biologic)
Many patients use injectable biologic medications to manage various autoimmune conditions. These medications work by modifying the immune system, which can reduce your ability to fight infections and make you more susceptible to illness.
There are certain situations when it is advisable to pause your biologic medication – particularly if you have a suspected infection that may require antibiotics, or if you are already taking antibiotics for a confirmed infection. If you’re feeling unwell and are unsure whether to take your medication, it’s always best to contact your clinical team for guidance.
For patients on non-biologic injectable medications: if you feel unwell or suspect an infection, please consult your GP to determine whether antibiotics are needed. While this usually does not require stopping your medication, if you are feeling particularly unwell, it may be advisable to delay your dose – again, only on the advice of your clinical team.






